From Our Bureau
6th MAY 2020
The Corona Virus (CPVID-19) pandemic situation remained grim globally, with the confirmed cases across the world soaring to 35,88,773 and the death toll reaching 2,47,503 in the 215 affected countries and territories, according to the latest update from the World Health Organization (WHO).
Globally, European region continued to be the worst-hit, with 15,93,828 confirmed cases and 1,47,780 deaths. American region came next with 15,07,148 confirmed cases and 81,070 deaths. Eastern Mediterranean region reported 2,21,230 confirmed cases and 8,290 deaths.
Western Pacific region’s tally stood at 1,54,884 confirmed cases and 6,327 deaths. South-East Asia region recorded 76,998 confirmed cases and 2,821 deaths and African region witnessed 33,973 confirmed cases and 1,202 deaths. WHO Risk Assessment at global level remained very high.
It has been 20 years since the inception of the Global Outbreak Alert and Response Network (GOARN), a close WHO partner which has responded to emergencies in 85 different countries, including the COVID-19 pandemic.
The WHO Regional Director for the Americas, Dr. Carissa F. Etienne, warned that reducing social distancing measures “too soon could accelerate the spread of the virus and open the door for a dramatic upsurge or for spread to adjacent areas.”
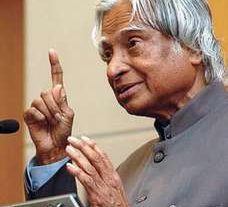
In the media briefing, WHO Director General Dr Tedros Adhanom Ghebreyesus said that “more than 3.5 million cases of COVID-19 and almost 250,000 deaths have now been reported to WHO. Since the beginning of April, an average of around 80,000 new cases have been reported to WHO every day. But these are not just numbers – every single case is a mother, a father, a son, a daughter, a brother, sister or friend.”
“Although the number of cases reported from Western Europe is declining, more cases are being reported every day from Eastern Europe, Africa, South-East Asia, the Eastern Mediterranean and the Americas. However, even within regions and within countries we see divergent trends. Every country and every region needs a tailored approach. But the impact of the pandemic goes far beyond the numbers of cases and deaths,” he observed.
“Around the world, the pandemic has caused severe disruption to essential health services – including to community-based health care. Although professional health workers like doctors and nurses play crucial roles, in many countries trained members of the community play a vital role in delivering essential health services like vaccination, pre-natal screening, and the detection, prevention and management of many diseases,” he added.
Today, WHO, UNICEF and the International Federation of the Red Cross have published guidance for countries on how to maintain community-based health care in the context of COVID-19. It includes practical recommendations for countries on sustaining essential services at the community level, leveraging community health workers for the response to COVID-19 while keeping them safe, and advice for how to adapt services for specific diseases and age groups. For example, it suggests using telemedicine wherever possible, and leaving insecticide-treated nets for malaria at the door of households, instead of asking people to collect them from a central location.
“It’s also vital that countries pay careful attention to the most vulnerable members of their societies. Crises can exacerbate existing inequalities, which is demonstrated in higher rates of hospitalization and death among certain populations in many countries. We must address this now and in the long-term by prioritizing diagnosis and care for those who are most at risk. This is not only the right thing to do, it’s the smart thing to do. We cannot end the pandemic until we address the inequalities that are fueling it, the WHO Director-General pointed out.
“Today’s guidance complements the United Nations framework for the socio-economic response to COVID-19, published last week. The framework lays out a “recovery roadmap” for countries to protect lives and livelihoods, and get businesses and economies up and running again as soon as possible. Importantly, the framework takes a “health first” approach, recognizing that strong and resilient health systems must be the foundation of recovery in all countries.
“As more and more countries consider how to ease so-called lockdown restrictions, I want to reiterate the six criteria that WHO recommends countries consider: First, that surveillance is strong, cases are declining and transmission is controlled; Second, that health system capacities are in place to detect, isolate, test and treat every case and trace every contact; Third, that outbreak risks are minimized in special settings like health facilities and nursing homes; Fourth, that preventive measures are in place in workplaces, schools and other places where it’s essential for people to go; Fifth, that importation risks can be managed; And sixth, that communities are fully educated, engaged and empowered to adjust to the `new norm.’”
“The risk of returning to lockdown remains very real if countries do not manage the transition extremely carefully, and in a phased approach,” he added.
“The pandemic has highlighted the importance of strong national and sub-national health systems as the foundation of global health security and universal health coverage. Strong and resilient health systems are the best defence not only against outbreaks and pandemics, but also against the multiple health threats that people around the world face every day.
“And yet, on current trends, more than 5 billion people will lack access to essential health services by 2030 – including the ability to see a health worker, access to essential medicines, and running water in hospitals. Gaps like these don’t just undermine the health of individuals, families and communities; they also put global security and economic development at risk.
“The world spends around US$7.5 trillion on health each year – almost 10 percent of global GDP. But the best investments are in promoting health and preventing disease at the primary health care level, which will save lives and save money. Prevention is not only better than cure, it’s cheaper, and the smartest thing to do.
“The COVID-19 pandemic will eventually recede, but there can be no going back to business as usual. We cannot continue to rush to fund panic but let preparedness go by the wayside.
As we work on responding to this pandemic, we must also work harder to prepare for the next one. Now is an opportunity to lay the foundations for resilient health systems around the world, which has been ignored for too long. That includes systems to prepare, prevent and respond to emerging pathogens.
“If we learn anything from COVID-19, it must be that investing in health now will save lives later. History will judge all of us not only on whether we got through this pandemic, but also on the lessons we learned and the actions we took once it was over. Before I end I will repeat something I have said many times: The antidote for this pandemic is national unity and global solidarity. Together, we will defeat COVID-19,” he added. (eom)